Obstructive Sleep Apnea (OSA) is a fairly common sleep disorder that can have serious consequences if left untreated. If you’ve been diagnosed with sleep apnea, you may be considering surgery as a treatment option.
This guide will provide you with information you should know about surgery for sleep apnea, from the different types of procedures available to what you can expect during and after surgery.
What is Obstructive Sleep Apnea?
Symptoms and Risk Factors
Obstructive Sleep Apnea is a common disorder characterized by an interruption in breathing and shallow breaths caused by the upper airway’s tissues collapsing and blocking airflow. Common symptoms are loud or frequent snoring; abrupt awakenings; pauses in breathing; choking sensations; morning headaches; trouble staying asleep, and excessive daytime sleepiness.
Don’t take obstructive sleep apnea lightly – it’s an important medical condition that can directly lead to the development of other health issues, such as stroke, heart disease, diabetes, and even premature death. If you think that you may be suffering from this disorder, seek help from your doctor for proper diagnosis and treatment.
Treatments For Obstructive Sleep Apnea
Achieving success with OSA treatment is not always easy, as many people suffering from sleep disorders are in good health. Furthermore, aside from surgery–which is permanent–the various possible therapies require regular compliance; these treatments won’t work if they’re left on a bedside table or tucked away in the back of your closet! As such, successful OSA management may necessitate more than one solution tailored to the individual’s needs and lifestyle.
1. CPAP
CPAP, or continuous positive airway pressure, is the most common treatment for sleep apnea. A CPAP machine uses a mask that fits over your nose and mouth and delivers a steady column of air that keeps your airway open while you sleep.
2. Surgery
Surgery is an option for people with sleep apnea who cannot tolerate CPAP or who do not respond to other treatments. Several types of surgery can be effective in treating sleep apnea, but they all carry some risks.
3. Oral Appliances
Oral appliances are dental devices that look like night guards they are worn in the mouth during sleep to position the jaw slightly forward and provide tissue tone that keeps the airway from collapsing during sleep.
Examples of these devices are Silent Night, EndSnorZ, and TAP.
For those with mild to moderate sleep apnea who cannot tolerate CPAP or have not had luck with other treatments, mandibular advancement devices are a great option. In fact, one study of 58 adult patients found that 31% experienced at least 50% AHI reduction when using the appliance – an impressive result! Not only do they affect the reduction in AHI but they are also well tolerated by most patients.
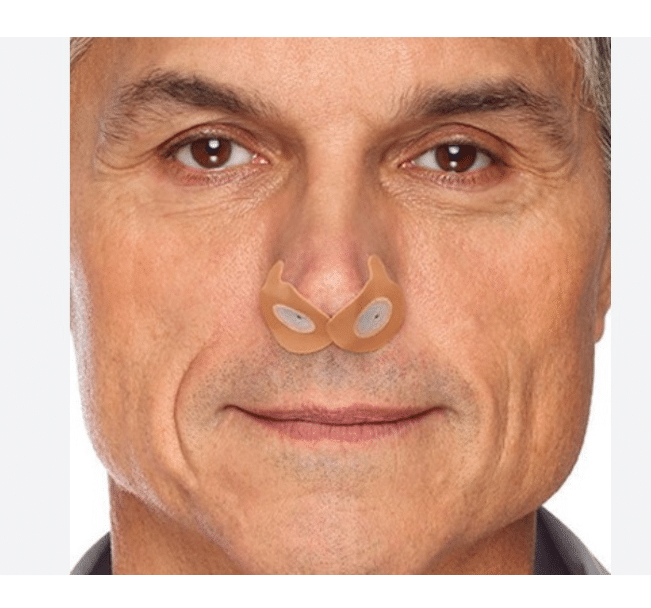
4. Nasal Resistors
Nasal resistors are small devices that are inserted into the nostrils to provide slow exhalation and expiratory positive airway pressure to the airway that keeps the airway from collapsing. These devices are an option for those with mild to moderate sleep apnea who cannot tolerate CPAP or have not had luck with other treatments.
5. Weight Loss
Shedding even a few pounds can have dramatic effects on your sleep apnea and overall health, especially if you are overweight or obese.
Excessive fat around the abdomen compresses one’s chest wall, diminishing lung volume which consequently reduces airflow.
It has been found that an increase in 10% body mass index (BMI) is connected to a 6X increase in Obstructive Sleep Apnea (OSA) risk.
Therefore, weight loss is an important tool for improving sleep apnea symptoms and leading healthier lives.
6. Behavioral Changes
Making certain behavioral changes can also help to treat sleep apnea. These changes include avoiding alcohol and smoking, sleeping on your side instead of your back, and avoiding sedatives before bedtime . Additionally, maintaining a regular sleep schedule and avoiding caffeine in the evening can also help.
Finally, elevating the head of your bed by four to six inches can reduce nighttime snoring and improve airflow.
Surgery for OSA
Surgery is an option that may be explored if other treatments for sleep apnea don’t work or are not well tolerated. These may range from relatively minor procedures, such as removing the tonsils or deviating the nasal septum, to much more complicated operations like a tracheostomy or Maxillomandibular advancement surgery (MMA).
While these procedures can provide relief from disrupted sleep and boost the overall quality of life, they also come with their own risks. This includes infection, excessive bleeding, and post-surgery pain or discomfort.
Generally, surgery should only be utilized as a last resort for treating obstructive sleep apnea due to its intrusive nature and uncertain effectiveness in the long term. Because OSA affects one or more upper airway pathways, surgeons have developed a multilevel single-stage procedure with an impressive success rate of 60%. This protocol has drastically enhanced surgical outcomes; though unfortunately it still requires multiple surgeries which can be daunting for some patients.
Nevertheless, it remains an important option for clinicians and patients trying to manage sleep apnea.
Sleep Apnea Surgical Procedures
Uvulopalatopharyngoplasty (UPPP)
Uvulopalatopharyngoplasty, otherwise known as UPPP, is a surgical procedure performed to reduce obstruction in the upper airways. This is typically done to treat sleep apnea and snoring, or for more severe cases of OSA (Obstructive Sleep Apnea). It involves removing soft tissue from the back of the throat, such as all or part of the uvula, parts of the soft palate and surrounding tissues, and any remaining tonsils/adenoids. Depending on the severity of a patient’s OSA, it can be done on its own or with other treatments. UPPP is a minimally invasive procedure with considerable success in many patients.
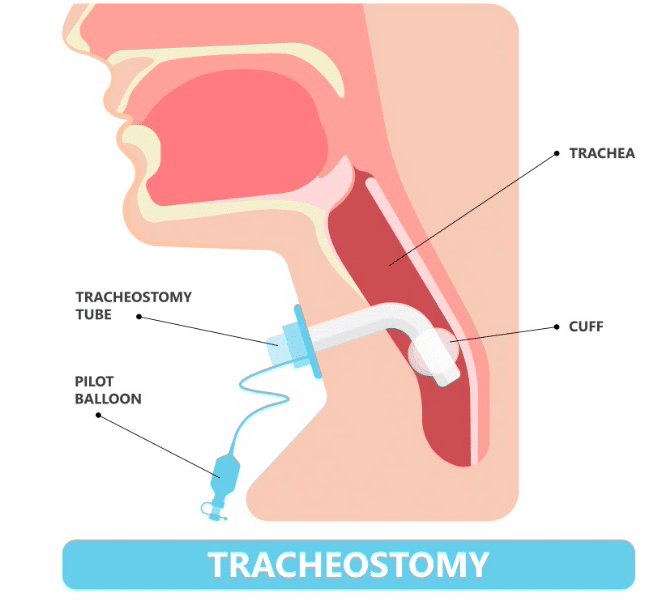
Tracheostomy
Tracheostomy is an important surgery to be aware of if you suffer from severe obstructive sleep apnea (OSA). It is used when other treatments including breathing devices and lifestyle changes have failed, or if another surgical treatment won’t work for you.
This procedure involves a permanent opening in the throat that connects to the windpipe. A valve is inserted in the opening.
In this method, the valve is kept closed during the day which allows normal speech and breathing; however, at night, the valve is opened so air can bypass the blockage in the airway and into your lungs more easily as you sleep.
Tracheostomy is very invasive however studies have shown that this surgery is almost always successful when treating severe sleep apnea.
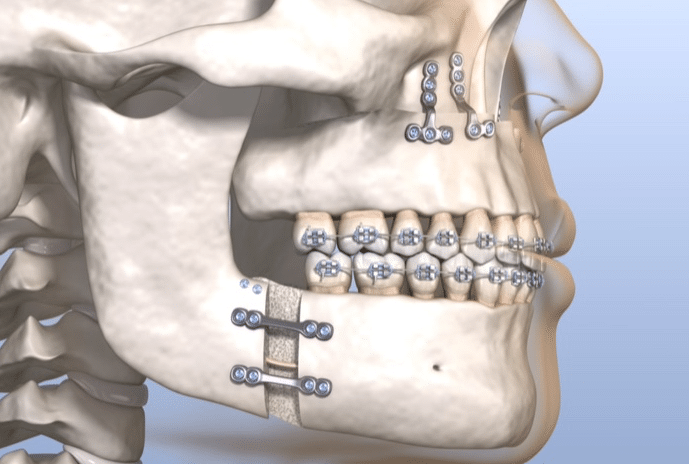
Maxillomandibular Advancement (MMA)
Maxillomandibular advancement surgery (MMA) is an effective treatment for obstructive sleep apnea (OSA). In MMA, bones of the upper and lower jaw are repositioned to open up the airway, along with suspending attached pharyngeal airway muscles into an anterior position which increases soft tissue tension.
What makes MMA unique among treatments for sleep apnea is its involvement in all areas of the airway – ranging from the nasal cavity down to the hypopharynx. The success rate is quite high as more than half of those with severe sleep apnea can achieve elimination (apnea-hypopnea index less than 5).
Genioglossus advancement and midline glossectomy/base of tongue reduction
Genioglossus Advancement (or tongue base advancement) is a viable treatment option for those with blocked airways due to the tongue blocking their airway. The surgery is quite successful, with reported rates as high as 78%, and involves manually moving the genioglossus muscle forward so it enables an individual’s airway to open more easily.
If patients are contraindicated for Genioglossus Advancement, surgeons may instead opt for a midline glossectomy or tongue base reduction. This procedure uses lasers or robots to carefully remove excess tissue from the base of the tongue and reduce tongue size and increase the size of the airway. Both of these procedures offer a potential benefit to patients who suffer from sleep apnea.
Lingual tonsillectomy
Lingual tonsillectomy is a surgical procedure involving the removal of the lingual tonsil to open up the airway behind the tongue. The procedure is used primarily for those suffering from sleep apnea and who have large tongues that compress their airways.
This surgery is performed in an operating room under general anesthesia, without any incision through the skin, instead working exclusively through the open mouth.
Once complete, this procedure yields larger airways and improved breathing for those previously affected by sleep apnea or obstructed breathing caused by an overly large tongue.
Hypoglossal Nerve Stimulation
Hypoglossal Nerve Stimulator (HNS), developed by Inspire Medical Systems, is an implantable medical device that works within the body to reduce sleep apnea by electrically stimulating the hypoglossal nerve which causes the tongue to move. This stimulation is timed with breathing, opening air passages, and relieving the upper airway obstruction caused by sleep apnea.
Hyoid Suspension
Your doctor may recommend hyoid suspension surgery to secure the hyoid bone forward and stabilize the airway.
The hyoid bone is a small bone located in the neck that is supported by what is known as the Adam’s apple.
If a patient has a larger-than-normal tongue or weak tongue muscles, this procedure can help reduce snoring and sleep apnea by preventing the tongue from collapsing into the airway at night.
It should be noted that sometimes hyoid suspension surgeries are done in combination with other procedures such as genioglossus advancement for more complicated cases.
Offer a step-by-step guide to preparing for sleep apnea surgery
Surgery for sleep apnea (OSA) requires some advance preparation. Depending on the procedure and the individual’s circumstances, surgery might involve the nose, soft palate, tongue, and/or jaw, with the potential to even include an implant like Inspire for hypoglossal nerve stimulation.
One important way to prepare is to learn about where sleep apnea surgery takes place; most likely it will be at a hospital or outpatient center.
Additionally, have a clear idea as to what you should wear and bring to the surgery so that you are comfortable once there.
Finally, be aware of any adjustments in terms of food, drink, or pre-operative medications that may be necessary—ask your doctor for guidance in this regard if needed. Surgery for OSA can require some upfront forethought and planning; following these steps can ensure things go more smoothly on the day of your surgery.
Post Operative Considerations
In most cases, full recovery from surgery for sleep apnea is expected within several months.
In some cases, minor procedures within the nose may have minimal pain or symptoms and can be tolerated within days following surgery.
In contrast, surgery involving the throat or tongue may have a longer recovery period that improves over weeks, while jaw advancement surgery could take up to one month or longer to return to baseline.
After two months of healing, it’s important to reassess the condition to determine the impact of the procedure on sleep apnea symptoms, which can require a repeat sleep study (either a home test or an in-center diagnostic polysomnogram).
If sleep apnea has resolved after the procedure, the residual Apnea-Hypopnea Index should be lower than 5 and oxygen saturation higher than 90%, which indicates successful treatment. In terms of daily activity post-surgery, it will vary depending on the type of procedure performed, any complications arising from it as well as individual pain tolerance and health status.
Long-term Benefits
Sleep apnea surgery is an important and effective treatment option that many don’t recognize or pursue, often for good reason.
But when successful, surgery is a permanent solution that can feel like a cure, not a treatment.
Surgery can offer a range of long-term benefits, providing patients with relief from daytime sleepiness, improved sleep quality, and greater overall well-being.
This in turn can lead to enhanced cognition, better moods and concentration, more energy, and even better overall health through reduced risk for diabetes, heart attack, and stroke.
In short, successful surgery can significantly improve a patient’s quality of life over the long term.
Conclusion
Surgery is a viable treatment option for those with sleep apnea who cannot tolerate continuous positive airway pressure (CPAP) therapy.
There are four main types: maxillomandibular advancement, uvulopalatopharyngoplasty, Hypoglossal Nerve Stimulation, and tongue reduction surgery.
Before having any sort of elective surgery, you must do your research and talk to your physician to ensure that the procedure is right for you.
This guide provides a brief overview of surgery for sleep apnea and what you can expect before, during, and after the procedure. If you think that surgery might be the right treatment option for you, talk to your physician about the next steps for treating your sleep apnea.