Sleep apnea is by definition an airflow condition. Respiration or airflow, with effort (Obstructive Sleep Apnea or OSA) or without effort (central sleep apnea, CSA), is the key attribute and often gets lost in the discussion of sleep apnea treatment. Discussions about airway caliber, jaw position or airway patency are all secondary to measured airflow and respiratory effort.
In order for a patient to respond well to any sleep apnea therapy it is critical that the patient have sufficient lung function to breathe properly on their own. If a patient has Asthma, Chronic Obstructive Pulmonary Disease (COPD) or Obesity the chances of them having sleep disordered breathing symptoms is very high. The definition of sleep apnea is a cessation of airflow for 10 seconds or more. The Apnea Hypopnea Index includes shallow breaths or Hypopneas into the mix which makes managing patients with restrictive or obstructive lung disorders even more difficult. COPD affects approximately 20 million people in the United States and is the nation’s third leading cause of death.
Xavier Soler, MD, PhD, Assistant Professor of Medicine, Pulmonary and Critical Care Division, University of California San Diego, reports in his national COPD foundation Blog that:
“Patients with severe COPD commonly exhibit abnormal sleep like insomnia contributing to chronic fatigue, daytime sleepiness. Additionally, medications used to treat COPD, such albuterol or prednisone may affect sleep quality. A nocturnal reduction of nocturnal oxygen levels commonly seen in patients with COPD can have profound effects and contribute to long-term sequelae, producing arrhythmias, myocardial stress, and, possibly, lower survival.”
The connection between OSA and COPD is very close Dr Soler goes on…
“OSA occurs in about 10 to 15% of patients with COPD, a condition referred to as the “overlap syndrome”. Although the prevalence of OSA is similar in patients with COPD as in the general population, individuals with both conditions without CPAP treatment have an increased risk of death and more hospitalizations from acute exacerbations.”
As clinical teams take on the management of sleep disordered breathing they will encounter patients with COPD, Asthma and Obesity related obstructed breathing or shortness of breath (dyspnea). Is it reasonable to assume that a patient with reduced spo2 and obstructed or shallow breathing patterns while awake, will also have these conditions while asleep? If so, how should the clinician rule out these conditions to adjust expectations or manage sleep disordered breathing based on each patient’s normal values?
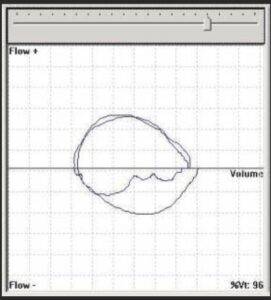
Lung disorders can be objectively identified and managed with tools like the Asthma Control test questionnaires and Spirometry (CPT 94375) . The most common pulmonary function tests are based on the Forced Vital Capacity (FVC) maneuver taken using a spirometer. Flow-volume curves are used to present lung function data. Normal values for spirometry tests have been compiled into tables called normograms which are based on age, height, sex and race. In adults, a Forced Expiratory Volume in one second (FEV1) that is lower than 80% of predicted value is considered abnormal. The department of pulmonology at Hopital de Hautepierre in Strasbourg France conducted a study called “Association of Chronic Obstructive Pulmonary Disease and Sleep Apnea Syndrome”, where patients with known sleep apnea were tested with a spirometer and 11% were found to have an FEV1 <60%. These patients were older and all were male. It is interesting to note that BMI in Overlap patients was identical to the non overlap patients. In other words the collection of FEV1 data would be very useful in managing this patient population.
FEV1 is the amount of air that a patient can forcefully exhale through a spirometer in 1 second and is the most standardized indicator of obstructive impairment. This measurement is of flow however it is reported as a volume. This is a coaching dependent maneuver which requires the patient to take a deep breath in and blast out as much air as they can as fast as possible for at least six seconds. The data generated are in Liters and the 1 second value is presented as a Flow Volume Loop (FVL). The FVL will show peak expiration and reduction in flow over time with full inspiration at the bottom of the loop. The shape of the curve will show clearly obstruction or restrictive patterns. Collection of Flow volume loops is a standardized lung function test reported in awake patients.
Once base flow characteristics for the individual patient is established, then a Flow Volume loop can be used to track the effectiveness of medicines and therapies in improving inspiratory or expiratory flow volumes. During sleep these flow volume loops can be collected during tidal breathing. They are used to calibrate therapies in the same fashion. The shape of the flow volume loops are diagnostic and can be used as a guide to avoid over and under titrations of sleep therapies.
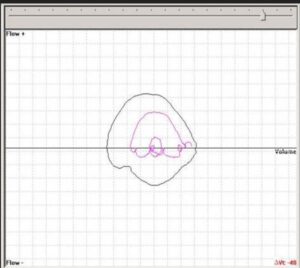
Inspiratory flow limitation
In the sleep lab the sleep technician can identify a biologic normal breath while the patient is awake and relaxed. By saving the loop and comparing loops while cpap is being titrated or calibrated the saved loop can be compared to treated breaths. The patient in fact becomes their own biologic standard for calibration of their personal sleep treatment.
The technology used to make this measurement is Respiratory Inductance Plethysmography (RIP) and is listed as a “ideal for identification of respiratory effort”, by the AASM. The real advantage of avoiding over and under titrations is that patient outcomes improve.
As we take on the treatment of sleep disordered breathing we should consider that the patient may in fact present with “the Overlap Syndrome”. It is unclear what level of severity the co existing conditions of sleep apnea and COPD start to contribute to clinical risk. It is clear that there is enough data indicating that the conditions occur together to evaluate lung function in patients presenting for sleep therapy. In my opinion this is particularly true for patients who are non compliant with other therapies indicating that they may have a confounding issue complicating their sleep condition.
Application of sleep therapies requires diagnostic procedures that isolate and quantify the disease. Where possible the same diagnostic procedures should be used to calibrate or manage treatment. The inclusion of spirometer testing is indicated to evaluate lung function in the wake patient to exclude the Overlap Syndrome. The use of flow volume loops during sleep to measure Upper Airway Resistance Syndrome and to calibrate sleep apnea treatments, to the patients biologic norms, during sleep are also an important tool for improved patient outcomes.