Obstructive sleep apnea (OSA) and chronic obstructive pulmonary disease (COPD) are very common conditions. Prevalence of both COPD and OSA in adults over 40 is thought to be between 5 and 10%. Chances of a patient suffering from both conditions is relatively high – roughly 1 in 200 adults over 40.
Both OSA and COPD cause a severe drop in blood oxygen during sleep. They both can lead to increased risk of disability and early death.
Since they are often found together, the big question is:
Does obstructive sleep apnea syndrome (OSA) cause chronic obstructive pulmonary disease (COPD) or, does COPD cause OSA?
In this blog post we will examine how each condition affects blood oxygen level during sleep. We will also consider what patients experience when they occur together.
How does Breathing work?
Each of us have been breathing for our whole lives without really considering how breathing works or how miraculous the cardiovascular system is.
The average adult with normal health lungs takes 16 to 20 breaths per minute, children will often breathe a little faster than that.
As you take your next breath the “breathing pump muscles” of your respiratory system work together to pull air into your lungs. Your diaphragm contracts making the length and size of your chest cavity larger which makes your lungs bigger. Your intercostal muscles and neck muscles spread your rib cage and draw air into your lungs. Then the muscles contract and push carbon dioxide rich air out.
Upper Airway
Air is drawn into your lungs through your mouth or nose. It passes through your upper airway or pharynx. Your pharynx is made up of three distinct areas of soft tissue (collapsible).
- Nasopharynx (turbinates, uvula)
- Oropharynx (tonsils and base of the tongue)
- Hypo-pharynx
The upper airway not only provides a passage for breathing, this area also important because it warms and humidifies and filters inhaled air. The flexibility of the tissue of the upper airway is important because it also allows swallowing, speech and coughing.
Inhaled air then passes the voice box and enters the trachea. The trachea is very different from the upper airway It is defined by hard “C” shaped cartilage (not collapsible) and the softer wall of the esophagus that can expand and contract to allow swallowing.
The Lung
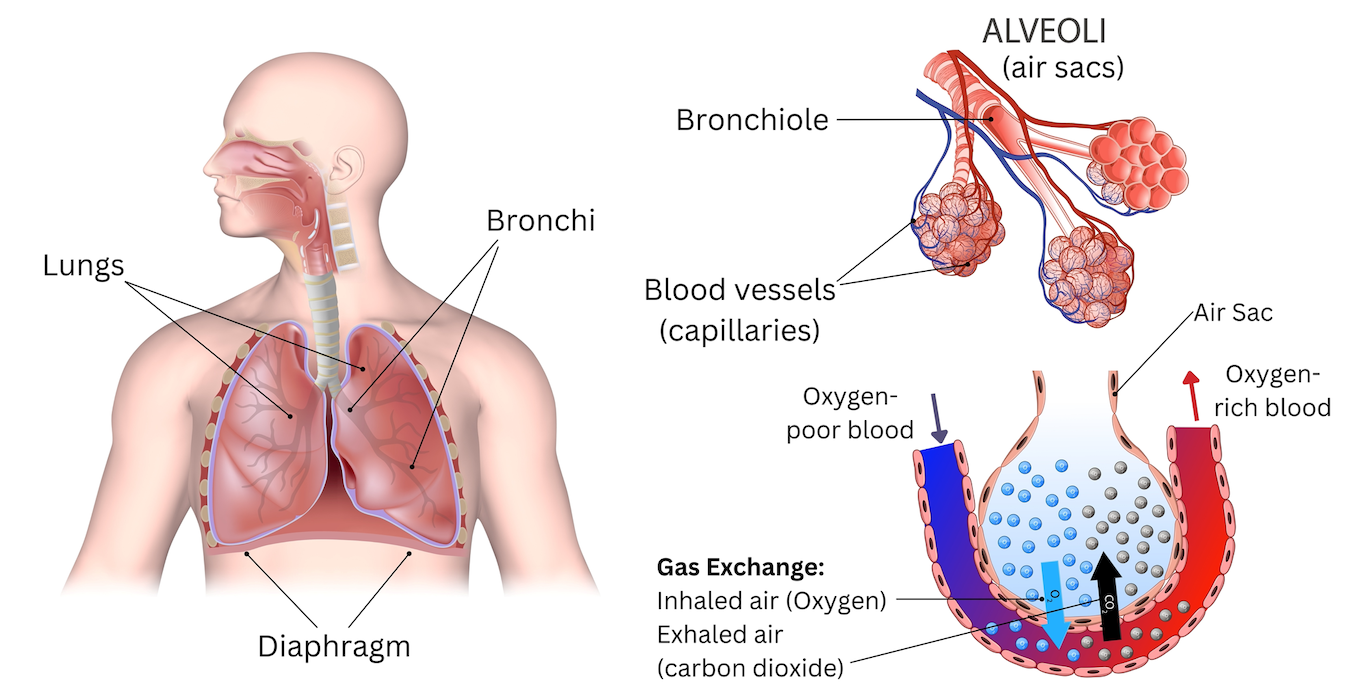
Within the lungs, the trachea branches into a left and right bronchus that are made of circular hard cartilage rings.
These branches further divide into smaller and smaller branches of lung tissue called bronchioles. They are tiny tubes that are about 1mm in diameter and do not have mucus creating cells.
The smallest bronchioles end in tiny air sacs. These are called alveoli they look like tiny bunches of grapes. Unlike grapes these tiny fragile structures are not individual balloons.
Alveoli inflate when a person inhales and deflate when they exhale. It is in the alveoli that oxygen transfers into the blood stream and carbon dioxide exits. This process is called gas exchange.
Gas Exchange
Gas exchange is when oxygen molecules transfer from the lung and attach to red blood cells, which travel back to the heart. At the same time, carbon dioxide molecules in the alveoli transfer into the lung and are exhaled completing one breath.
“It is widely reported that, a person at rest takes about 16 breaths per minute. This means we breathe about 960 breaths an hour, 23,040 breaths a day, 8,409,600 a year. The person who lives to 80 will take about 672,768,000 breaths in a lifetime. Since a person sleeps for a third of their life this 80 year old person will have taken 222,013,440 breaths while asleep (one third of their breaths). “
–Breathing is a 24 hour activity by Randy Clare, Dental Sleep Practice
Breathing and gas exchange allow the body to replenish oxygen in the blood and eliminate the carbon dioxide as waste. People who cannot breathe properly can become hypoxic which means blood oxygen level drops as a result of poor gas exchange. This is usually a result of fluid in the lungs, damage to the lung tissues or when the airway is obstructed.
Obstructive sleep apnea syndrome (OSAS) and chronic obstructive pulmonary disease (COPD), interrupt or inhibit gas exchange each in their own way.
The measure of nocturnal blood oxygen levels alone are not enough to be able to discern the difference between COPD and OSAS or both.
What is Sleep Apnea Syndrome?
Sleep Medicine defines Sleep Apnea as a breath hold, or cessation of breathing, during sleep for 10 seconds or longer. Sleep apnea is a condition that is defined by poor sleep quality and excessive daytime sleepiness.
There are 3 kinds of sleep apnea, obstructive sleep apnea, central sleep apnea and mixed sleep apnea.
- Obstructive Sleep Apnea
- Central Sleep Apnea
- Mixed Sleep Apnea
Obstructive sleep apnea (OSA) is when the patient tries to breathe, but the upper airway collapses obstructing airflow..
OSA is often associated with loud snoring because snoring is the sound a partially collapsed airway makes. Complete collapse of upper airway tissues obstructing the flow of air into the lung is OSA.
The patient labors to breathe against the obstruction until they gasp awake for a few breaths, then fall asleep again which allows the airway to collapse again. This cycle repeats over and over again resulting in fragmented sleep patterns, excessive daytime sleepiness and reduced quality of life.
The most widely accepted treatment for OSA is CPAP (continuous positive airway pressure). CPAP is a device the patient uses at night to blow a column of air into the airway to stop the collapse of soft tissues.
Central sleep apnea is a cessation of breathing that results from the brain not sending signals to the muscles of respiration that trigger a breath during sleep.
Mixed apnea is a condition that starts with the brain not signaling a breathe and then shifts to the patient struggling to breathe through a collapsed airway.
All three of these conditions are characterized by low nocturnal blood oxygen levels.
Obstructive Sleep Apnea
OSA is a very well known sleep disordered breathing pattern that is associated with loud snoring and, it is found in older patients who are obese and men are more susceptible to OSA than women.
Loud snoring and OSA can occur in most sleep stages but it is particularly acute during rapid eye movement (REM) stage of sleep.
Rapid eye movement sleep which is characterized by vivid dreams, most of the patients muscles are paralyzed (so they do not act out dreams). The effect on the relaxed collapsable soft tissue areas of your upper airway obstruct the airway.
One way to assess risk of sleep apnea is to be screened by a physician who may order an overnight sleep study, either in the hospital based sleep lab or with a home sleep testing device.
The STOP-bang Questionnaire is a generally accepted screening tool that is easy to take and easy to score yourself.
What is Chronic Obstructive Pulmonary Disease?
Chronic Obstructive Pulmonary Disease is a condition that is made up of several diseases that obstruct, block or restrict airflow into the lungs.
Breathing difficulties that fit into the category of obstructive airways disease include Chronic Bronchitis and Emphysema and Asthma.
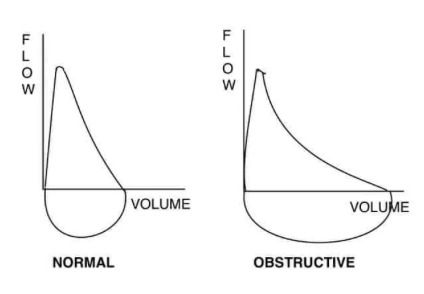
Chronic obstructive pulmonary disease is defined by reduced airflow into the lungs, generally because air does not flow freely in the lung.
Lung tissues are no longer flexible and cannot respond properly to breathing effort.
Alveoli structures are damaged or have collapsed.
Walls of airways become thick and inflamed (irritated and swollen)
Airways are clogged with mucus
Almost 15 million Americans have been diagnosed with COPD which is about 6% of the population.
It is reported by the CDC that 50% of people with restrictive pulmonary function are completely unaware of that they have the condition.
COPD is the fourth leading cause of death in America and is associated with smoking but is also linked to air pollution and respiratory infections.
The Centers for Disease Control and Prevention (CDC) reports that COPD is found more often among women in America. It is thought that women are more sensitive to tobacco and other indoor pollutants than men.
Symptoms of COPD include shortness of breath, swelling in the feet and ankles, smokers cough, elevated pulse rate, and blue lips and fingernails which is a sign of a drop in blood oxygen when awake and asleep.
How is Cigarette Smoking Related to COPD?
Cigar and Cigarette smoking or exposure to second hand smoke, is directly related to the breakdown of lung tissue and airway inflammation. It is important to note that 80% of patients with COPD die from COPD related symptoms.
It is striking that 25% of COPD deaths have never smoked. It is thought that the non smoking group of patients have been exposed to aerosol particulate in some other form.
How to get tested for COPD?
It is clear that COPD reduces lung function by damaging lung tissue, clogging up airways and blocking normal breathing pathways. Physicians order pulmonary function tests with a spirometer to confirm or monitor the progress of chronic obstructive airflow disease.
A spirometer is a device that measures airflow. Key measures of lung function are, how much air you can blow out in 1 second and how much air you can blow out in total also how long it takes to completely empty your lungs, the test takes about 20 minutes.
What is COPD, OSA Overlap Syndrome?
It is clear from the above, that COPD and sleep apnea syndrome are completely different diseases with different risk factors, at risk populations and testing protocols.
So the big question is “does sleep apnea cause COPD?”
“The short answer is no, they are two very different conditions with different treatments but with similar sequelae.”
Obstructive sleep apnea patients suffer from sleep fragmentation with each obstructive event a brief arousal occurs. This results in a disturbed sleep and excessive daytime sleepiness, when untreated sleepiness results in workplace accidents, car accidents and reduced quality of life. The implications of nocturnal oxygen desaturation for these patients in addition to the increased work of breathing are higher rates of obesity, diabetes, stroke, heart disease and early death.
Patients with COPD also have difficulties with sleep however their challenges are in falling asleep and staying asleep or insomnia. As the COPD patient passes through stages of sleep the reduced chest wall movement in REM makes breathing difficult due to narrow, scarred and damaged airways, excess mucus and chronic inflammation. The resulting nocturnal oxygen desaturation affects approximately 70% of patients with COPD. Difficulty breathing makes sleeping a challenge, also resulting in excessive sleepiness.
Clinicians who manage these two populations report that for patients who experience both COPD and OSA “overlap syndrome” the drop in oxygen saturation is more than when either condition is present individually.
The overlap in symptoms due to repetitive nocturnal oxygen desaturation events over and over through the night result in a chronic state of inflammation which can induce several conditions including:
high blood pressure
Stroke
Pulmonary Hypertension
Arrhythmias such as atrial fibrillation
Cognitive impairment
Increased risk of type 2 diabetes mellitus
Conclusion
In America it is estimated that 14% of adult men and 5% of adult women have obstructive sleep apnea. The undiagnosed OSA population is roughly 25 million people. A small number of OSA patients have “the overlap syndrome” which is coexisting chronic obstructive pulmonary disease COPD. When patients are diagnosed with COPD as their primary complaint it has been found that “overlap syndrome” has been present in 65.9% of cases.
Screening OSA patients for COPD requires different tools than a standard OSA protocol. For example STOP-band questionnaire is not sensitive or specific enough to identify these patients. Similarly it is recommended that home sleep testing is not recommended for at risk patients.
For patients with severe COPD it can be a real challenge to determine if the patients symptoms are a result of COPD exclusivley or overlap syndrome. It may be appropriate to screen all patients who present with severe COPD for OSA, Statistics certainly support that prevalence is high enough to make the effort worth while.
Treating these patients with continuous positive airway pressure (CPAP) with or without oxygen has been very successful when treating patients with overlap syndrome.
There is a very real impact on this patient population including quality of life implications and early death. It is critically important that clinicians and patients be aware of the risks of untreated Overlap Syndrome populations.