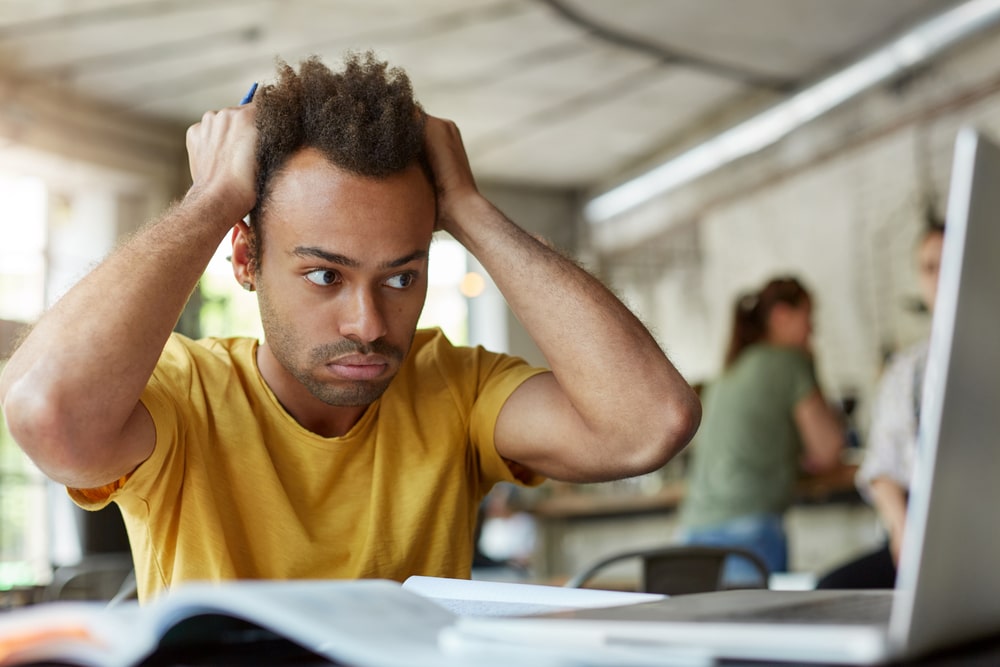
Do tension headaches or stress headaches plague you? Do they stop you from living life to its fullest or limit your ability to concentrate and be productive?
If so, you’re not alone. An estimated 20% of the adult population (1.4 Billion people) suffers from tension headaches regularly, yet the cause remains largely unresolved.
Through this blog post, you’ll learn how to make sense of these perplexing symptoms and understand why they persist even after trying lifestyle modifications and relief treatments that haven’t seemed effective until now.
We’ll explore key irritating factors to determine what triggers these common occurrences plus develop strategies for improving your overall health & well-being while also reducing localized pain & discomfort caused by tension headaches. So if it’s time for answers backed up with science – keep reading below!
What are tension headaches and what causes them?
Tension headaches are one of the most common types of headaches and they can be debilitating. They generally cause a dull ache or a band-like sensation of pressure and mild to moderate pain that wraps around the forehead and sometimes to the back of the head.
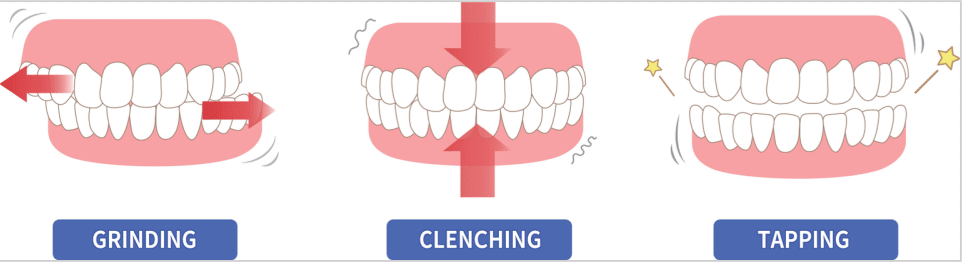
Chronic tension-type headache pain is usually caused by stress, anxiety, posture, or neck muscles that are contracted for too long. In addition, clenching your jaw or grinding your teeth (a condition known as bruxism) muscle contractions can also be to blame for tension headache symptoms.
How can you tell if you have a tension headache?
Headaches can be a real pain – literally. Sometimes it’s difficult to tell the difference between a headache, migraine, or medication overuse headache.
Knowledge of what to look out for makes it easier to spot the type of headache you’re experiencing.
Tension headaches typically feel like a dull aching hat band and don’t include flashing lights and uneven sight or nausea that sometimes come with migraines.
Conversely, overusing headache medicines can result in medication overuse headaches – also known as rebound headaches. If you’ve been having recurrent migraines directly after taking a pill for your pain, it’s very likely to be due to rebound headaches.
The last thing you want is to give yourself an even bigger headache! Of course, if in doubt speak to your doctor and have yourself checked out.
What are the symptoms of tension headaches?
Tension headaches are very common and can be diagnosed easily by noting the primary symptom: a constant, mild to moderate headache that is usually experienced as a “pressure” sensation rather than an intense throbbing pain.
Although it generally affects both genders equally, some studies suggest they occur more often in women between the ages of 18 and 50.
Frequent or severe headaches may also be triggered or made worse by stress, clenching, and grinding of the teeth, depression, and certain medications.
They may come on suddenly or build up gradually over several hours. While there is no definitive answer regarding possible genetic ties to tension headache pain, significant progress has been made in linking inherited genetics with other headache syndromes.
How do you treat tension headaches?
Dealing with chronic tension-type headaches can be a real headache. If you find yourself clenching your jaw throughout the day, or having pain that feels like a tight band around your head or neck and upper back pain, you are likely experiencing a tension headache or you have one coming on.
Fortunately, treating them doesn’t have to involve taking medication to relieve pain. In some cases, biofeedback and mindfulness exercises can help manage stress and reduce headache frequency and intensity over time.
Massaging sore muscles, icepacks, stretching, and exercise are also great methods to ease tension headache pain while they last. Whether it’s managing lifestyle habits or recognizing headache triggers and avoiding potential sources of stress – there are plenty of effective strategies to prevent tension headaches without drugs.
What preventative measures work to reduce your chances of getting a tension headache?
Avoiding the triggers of a tension headache is the best preventive measure you can take to reduce your chances of experiencing one.
1. Stress and tension headache is the most common type of headache. They are caused by muscle tension in the head, neck, and scalp muscles.
2. Tension headaches can be triggered by stress, anxiety, poor posture, or sleeping in an awkward position.
3. A tension headache can also be caused by eyestrain, teeth grinding, or jaw clenching.
4. Dehydration can also trigger tension headaches, as can skipping meals or not getting enough sleep.
5. Hormonal changes during menstruation can also cause a tension headache in some women.

6. Children and adolescents may also experience tension headaches due to stress from school or other activities.
7. Older adults may experience tension headaches due to arthritis or other age-related conditions.
8. People with migraine headaches may also experience tension headaches as a result of their condition.
9. Some medications can also cause a tension headache as a side effect, such as birth control pills, blood pressure medications, and antidepressants like Selective serotonin reuptake inhibitors (SSRIs) which are often used with cognitive behavior therapy to treat depression.
10. If you suffer from chronic tension headaches, you may be diagnosed with a condition called chronic daily headache.
All in all, taking proactive steps towards preventing a tension headache will result in a more relaxed body overall!
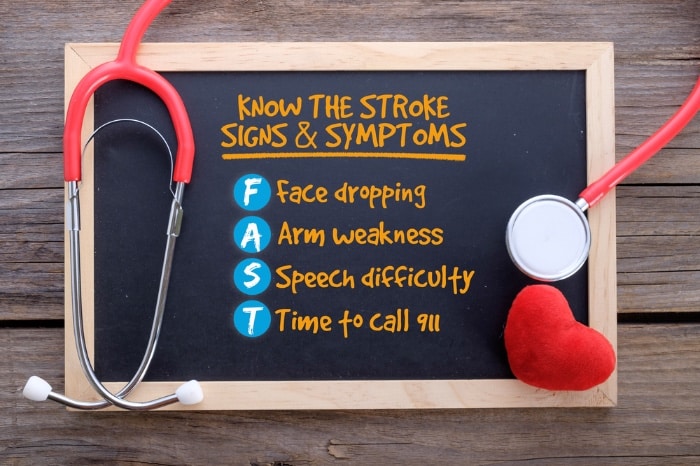
How to know if a tension headache is an emergency (e.g., stroke, seizure, etc)?
If you’re experiencing the worst headache you have ever experienced or a sudden intense headache, that comes on like a thunderclap, coupled with memory loss, confusion, or changes in vision or speech, it may be a sign of a stroke or seizure.
9 signs and symptoms of a stroke.
1. Sudden onset of symptoms: A stroke usually occurs suddenly, and the symptoms can vary depending on which area of the brain is affected.
2. Numbness or weakness of the face, arm, or leg: This is often the most noticeable symptom, as it can cause one side of the face to droop or one arm or leg to become weak or paralyzed.
3. Confusion or trouble speaking: A stroke can cause difficulty understanding others or trouble speaking clearly.
4. Trouble seeing in one or both eyes: A stroke can cause vision problems in one or both eyes, such as blurred vision or complete blindness.
5. Trouble walking: A stroke can cause difficulty walking, staggered gait, or complete paralysis.
6. Dizziness: A stroke can cause a feeling of dizziness or lightheadedness.
7. Loss of balance: A stroke can cause a loss of balance and coordination.
8. Severe headache: A stroke can cause a sudden and severe headache that is often described as a “thunderbolt” headache.
9. Loss of consciousness: A stroke can cause unconsciousness or coma.
What to do if you suspect someone is having a stroke
A stroke is not a headache but “stroke” is an increasingly common yet dangerous health issue in the United States, and it’s important to know what signs to look out for.
It is estimated that 80% of strokes can be prevented with proper education and awareness. Stroke is the fifth most common cause of death and a leading cause of disability in America; about 795,000 occur each year – 610,000 of those being new occurrences and 185,000 being recurrent.
If any combination of the above symptoms arise without warning in someone around you, it’s important to act fast by calling 911 and getting them medical attention immediately.
Conclusion
Tension and stress headaches are no fun, but thankfully there are things you can do to lessen their frequency and severity. Be careful to listen to your body and identify any headache triggers so you can prevent tension headaches in the future. Keeping a headache diary is an excellent way to more easily and accurately communicate with your Dr if that becomes necessary. If you found this blog helpful, please leave a comment below letting us know how we did. And if you have any suggestions for future article topics, be sure to let us know that too!
Resources
- The International Headache Society
- National Headache Foundation
- The American Migraine Foundation
- The American Stroke Foundation