Pregnancy is a time of many changes, including changes in sleep patterns. Many pregnant women struggle to get a good night’s sleep, but for around 20% of them, the problem may be obstructive sleep apnea (OSA).
This condition affects almost 30 million people in the United States and causes breathing problems during sleep due to airway obstruction. The throat may collapse during sleep due to a variety of factors, including excess weight, throat anatomy limitations, and hormonal changes.
Women often ask “can pregnancy cause sleep apnea?”
Pregnant women are at an increased risk for OSA due to the changes that their bodies undergo during pregnancy. However, the condition often goes undiagnosed or untreated.
This is because the symptoms of OSA can be similar to common pregnancy side effects like headaches, heartburn, morning nausea, and emotional changes like anxiety and depression.
Sleep apnea during pregnancy can have serious health consequences for both the mother and the baby. It can increase the risk of high blood pressure, preeclampsia, gestational diabetes, premature delivery, and complications during anesthesia or a longer labor.
According to data from the National Institutes of Health, the risk of death prior to discharge after delivery is 2.47% with OSA compared to 0.13% in patients who do not have OSA.
“Untreated sleep apnea in pregnancy can lead to significant maternal and fetal morbidity, emphasizing the need for early identification and management of this disorder.”
American Journal of Obstetrics and Gynecology, November 2018.”
Thankfully, research has shown that both continuous positive airway pressure (CPAP) therapy and oral appliance therapy (OAT) are safe and effective ways to reduce these risks before, during, and after pregnancy.
CPAP therapy involves using a machine to deliver a constant stream of air to keep the airway open during sleep, while OAT involves wearing a custom-made oral appliance that repositions the lower jaw and tongue to maintain an open airway.
Both therapies can help to ensure that both the mother and the baby get the oxygen they need during sleep.
It’s important to recognize that sleep is a crucial component of a healthy pregnancy, and sleep apnea can significantly impact a pregnant woman’s health and well-being.
If you’re pregnant and having trouble sleeping or experiencing any of the symptoms of OSA, it’s important to speak with your healthcare provider. They can help you determine if you’re at risk for OSA and recommend appropriate treatment options, which may include CPAP therapy, OAT, or a combination of both.
This blog post will explore the link between pregnancy and sleep apnea and provide valuable information on the causes, symptoms, diagnosis, treatment, and management of this condition.
What is Sleep Apnea?
Sleep apnea is a sleep disorder that occurs when a person’s breathing repeatedly stops and starts during sleep.
There are two types of sleep apnea: obstructive sleep apnea (OSA) and central sleep apnea (CSA). OSA is the most common type of sleep apnea and is caused by a blockage of the airway.
CSA, on the other hand, is caused by a failure of the brain to signal the muscles to breathe.
OSA is the type of sleep apnea that is most commonly associated with pregnancy-related weight gain. The weight gain can cause excess fat to accumulate around the neck and throat, which can lead to airway obstruction during sleep.
Causes of Sleep Apnea in Pregnancy
As your pregnancy progresses, your body undergoes significant changes, including hormonal shifts. Estrogen and progesterone levels rise with each trimester, and progesterone specifically stimulates certain receptors in the brain that help drive your breathing and oxygen consumption.
However, as your body adjusts to these changes, you may start to experience symptoms of obstructive sleep apnea (OSA). OSA causes breathing issues during sleep due to repeated airway obstruction.
This is because your expanding uterus may restrict lung functional capacity by 20 percent on top of normal reductions typically seen during sleep, and your oxygen consumption increases approximately 20 percent.
This means that you’ll need to take more breaths per minute, even when your body should be relaxing.
At the same time, your body’s capillaries become engorged with blood, leading to increased fluid retention in the throat. This can cause the airway to narrow increasing airways resistance, especially at night when you’re sleeping.
This can lead to symptoms like pregnancy rhinitis and nosebleeds, which can also disrupt sleep, but are not related to OSA.
OSA symptoms tend to get worse as pregnancy progresses, which can be tricky since the symptoms mimic the side effects of pregnancy. Many pregnant women may go undiagnosed because of this.
Additionally, many women with OSA may not snore, but instead experience the ill effects of inadequate sleep like mood changes, anxiety, and general fatigue. Some patients may even confuse an apnea episode with having a nightmare.
Several factors can contribute to the development of sleep apnea during pregnancy. One of the primary causes is weight gain, which is particularly acute in the third trimester. Excess weight can cause airway obstruction during sleep, leading to sleep apnea.
Hormonal changes during pregnancy can also contribute to sleep apnea by causing inflammation and swelling in the airways.
If you’re pregnant and experiencing symptoms of OSA, it’s essential to speak with your healthcare provider. They can help you determine if you’re at risk for OSA and recommend appropriate treatment options, such as continuous positive airway pressure (CPAP) therapy or oral appliance therapy (OAT).
By taking proactive steps to manage sleep apnea during pregnancy, you can help ensure a healthy pregnancy and delivery for both you and your baby.
How Common is Sleep Apnea During Pregnancy?
Sleep apnea is a common condition during pregnancy, affecting approximately 1 in 5 pregnant women. The risk of developing sleep apnea increases with the amount of weight gained during pregnancy.
Women who gain more than 20 pounds during pregnancy have been found to be at higher risk of developing sleep apnea. That being said managing weight during pregnancy can be difficult consult with your Ob/Gyn or sleep medicine doctor about the best strategies to achieve a healthy weight.
Symptoms of Sleep Apnea
The symptoms of sleep apnea during pregnancy can vary but typically include:
- Loud snoring
- Pauses in breathing during sleep
- Gasping or choking during sleep
- Daytime fatigue or sleepiness
- Morning headaches
- Restless sleep
- Mood changes
It is essential to seek medical attention if any of these symptoms are present to receive proper diagnosis and treatment.
Diagnosis of Sleep Apnea
The diagnosis of sleep apnea during pregnancy involves a comprehensive evaluation of symptoms, medical history, and a sleep study. Sleep studies may be performed in a sleep lab or at home using portable monitoring devices.
The sleep study measures various parameters such as breathing, heart rate, oxygen saturation, and brain waves to determine the severity of sleep apnea. Based on the results of the sleep study, the healthcare provider will make a diagnosis and recommend appropriate treatment.
Treatment Options for Sleep Apnea During Pregnancy
The treatment options for sleep apnea during pregnancy depend on the severity of the condition. Mild cases of sleep apnea can be managed with lifestyle changes such as weight loss, positional therapy, and avoiding sleeping on the back.
Moderate to severe cases of sleep apnea may require:
Continuous Positive Airway Pressure (CPAP) Therapy
CPAP therapy is the most common treatment option for moderate to severe sleep apnea during pregnancy. CPAP therapy involves wearing a mask over the nose and/or mouth during sleep, which delivers a continuous stream of air to keep the airway open.

CPAP therapy has been shown to improve symptoms of sleep apnea during pregnancy, including snoring, daytime sleepiness, and fatigue. It can also improve maternal and fetal outcomes by reducing the risk of complications such as preeclampsia, gestational diabetes, and preterm birth.
“Continuous positive airway pressure (CPAP) therapy is the gold standard treatment for sleep apnea in pregnancy and has been shown to improve maternal and fetal outcomes.”
Sleep Medicine, March 2019.
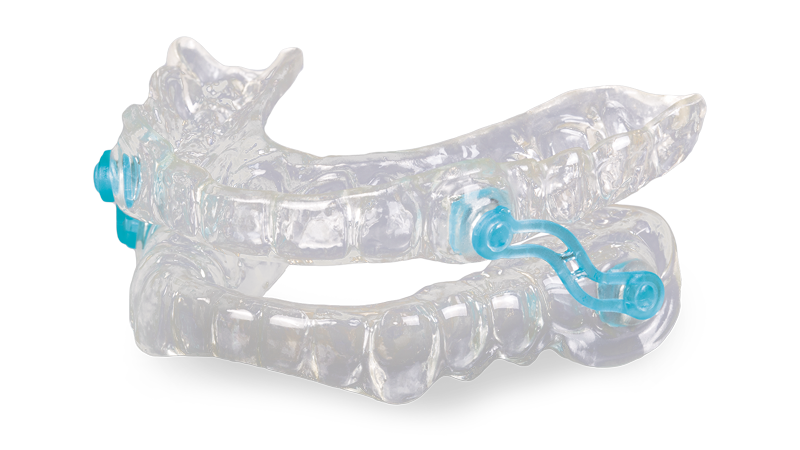
Oral Appliances
Mandibular advancement oral appliances (MADs) are commonly used for the treatment of obstructive sleep apnea (OSA) in patients with mild to moderate OSA or who cannot tolerate continuous positive airway pressure (CPAP) therapy.
MADs work by repositioning the mandible (lower jaw) forward during sleep, which supports the jaw helping to increase airway space and reduce airway resistance, preventing the collapse of the upper airway.
The appliance is custom-made for each patient and is worn like a mouthguard during sleep. MADs are a non-invasive and effective treatment option for mild to moderate OSA, and can also be used in combination with other therapies for more severe cases.
However, proper evaluation and fitting by a trained dental professional is crucial to ensure safety and effectiveness of the device.
Weight Loss
Weight loss can be an effective treatment option for sleep apnea during pregnancy, particularly for women who are overweight or obese. Losing weight can reduce the amount of fat around the neck and throat, which can improve breathing and reduce the severity of sleep apnea.
Weight loss can be achieved through a combination of diet and exercise. Pregnant women should work with their healthcare provider to develop a safe and effective weight loss plan.
Surgery
Surgery is generally not recommended as a treatment option for sleep apnea during pregnancy due to the potential risks to the mother and fetus. However, in rare cases where sleep apnea is caused by a physical obstruction such as enlarged tonsils or a deviated septum, surgery may be considered.
Lifestyle Changes to Manage Sleep Apnea during Pregnancy
Lifestyle changes can also be helpful in managing sleep apnea during pregnancy. These changes include:
- Sleeping position: Sleeping on your side rather than your back can help reduce the severity of sleep apnea. Using a pregnancy pillow to support your back and keep you in a side position can be helpful.
- Weight management: Maintaining a healthy weight during pregnancy is important for overall health and can also reduce the severity of sleep apnea. Eating a balanced diet and engaging in regular exercise can help manage weight.
- Avoiding alcohol and sedatives: Alcohol and sedatives can relax the muscles in the throat and make sleep apnea worse. Avoiding these substances can help improve sleep apnea symptoms.
- Nasal strips and saline sprays: Nasal strips (adhesive breathing strips) can help open up the nasal passages and improve breathing. Saline sprays can also help reduce nasal congestion and improve breathing.
- Oral appliances: Oral appliances such as MADs can be helpful in managing sleep apnea. These devices help reposition the jaw and tongue to support the jaw and keep the airway open.
- Quitting smoking: Smoking can increase the risk of sleep apnea and other pregnancy-related complications. Quitting smoking can improve overall health and reduce the severity of sleep apnea.
Importance of Seeking Medical Care for Sleep Apnea during Pregnancy
It is important for pregnant women with sleep apnea to seek medical care. Untreated sleep apnea can increase the risk of complications during pregnancy, such as preeclampsia and gestational diabetes. It can also increase the risk of preterm birth and low birth weight. Additionally, sleep apnea can lead to poor sleep quality, which can impact the mother’s mental health and well-being.
Pregnant women should speak with their healthcare provider if they are experiencing symptoms of sleep apnea. Healthcare providers can conduct a physical exam and may recommend a sleep study to diagnose sleep apnea. Treatment options can include lifestyle changes, continuous positive airway pressure (CPAP) therapy, and other interventions.
Questionnaires and Primary Care Physician Communication
Primary care physicians play an important role in identifying and managing sleep apnea during pregnancy. The American College of Obstetricians and Gynecologists recommends that pregnant women be screened for sleep apnea using a validated questionnaire at their first prenatal visit and at least once during the pregnancy.
Questionnaires such as the Berlin questionnaire and the Epworth Sleepiness Scale can be used to identify symptoms of sleep apnea. If a woman scores high on the questionnaire, she may be referred for a sleep study.
Healthcare providers should also be aware of the potential risk factors for sleep apnea in pregnant women, such as obesity, gestational diabetes, and preeclampsia. They can work with pregnant women to manage these risk factors and reduce the severity of sleep apnea.
Conclusion:
Sleep apnea is a common condition that can occur during pregnancy. It is important for pregnant women to be aware of the symptoms of sleep apnea and to seek medical care if necessary. Untreated sleep apnea can increase the risk of complications during pregnancy and can also impact the mother’s mental health and well-being.
Primary care physicians play an important role in identifying and managing sleep apnea during pregnancy. Pregnant women should be screened for sleep apnea using a validated questionnaire at their first prenatal visit and at least once during the pregnancy.
Treatment options for sleep apnea during pregnancy include lifestyle changes, continuous positive airway pressure (CPAP) therapy, and other interventions. Women should work with their healthcare provider to determine the best treatment plan for their individual needs.
Overall, early detection and treatment of sleep apnea in pregnant women is crucial for the health of the mother and the baby.
References
- Facco, F. L., Kramer, J., Ho, K. H., & Zee, P. C. (2010). Sleep disturbances in pregnancy. Obstetrics and gynecology clinics of North America, 37(4), 571-581.
- Franklin, K. A., Holmgren, P. A., & Jonsson, F. (2000). Snoring, pregnancy-induced hypertension, and growth retardation of the fetus. Chest, 117(1), 137-141.
- Izci, B., Vennelle, M., Liston, W. A., & Dundas, K. C. (2006). The effects of maternal sleep-disordered breathing on offspring birth weight and respiratory health. Sleep, 29(10), 1393-1396.
- Louis, J. M., Koch, M. A., Reddy, U. M., Silver, R. M., Parker, C. B., & Willinger, M. (2013). Predictors and timing of sleep-disordered breathing in pregnancy. Obstetrics and gynecology, 122(4), 753.
- Manchanda, S., & Rakkar, M. (2014). Sleep apnea in pregnancy. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine, 10(4), 425.
- O’Brien, L. M. (2012). Sleep disorders in pregnancy. Obstetrics and gynecology clinics of North America, 39(3), 401-417.
- Pamidi, S., Marc, I., Simoneau, G., Lavigne, L., & Olha, A. (2012). Maternal sleep-disordered breathing and adverse pregnancy outcomes: a systematic review and metaanalysis. American journal of obstetrics and gynecology, 207(5), 389-398.
- Pien, G. W., & Pack, A. I. (2007). The relationship between obstructive sleep apnea and hypertension. Current hypertension reports, 9(3), 204-210.
- Reddy, U. M., Davis, J. M., Ren, Z., Greene, M. F., & Consortium, E. S. (2012). Epidemiology of sleep disorders during pregnancy. Sleep, 35(3), 325-331.
- Young, T., Peppard, P. E., & Gottlieb, D. J. (2002). Epidemiology of obstructive sleep apnea: a population health perspective. American journal of respiratory and critical care medicine, 165(9), 1217-1239.