Obstructive sleep apnea and high blood pressure are two common conditions that affect millions of people worldwide. While these conditions may seem unrelated, recent research has found a strong link between disturbed sleep and blood pressure.
Sleep apnea is sleep disordered breathing characterized by repeated pauses in breathing during sleep. These pauses can last for a few seconds to a few minutes and can occur many times throughout the night, leading to poor sleep duration and excessive daytime sleepiness.
On the other hand, high blood pressure, also known as hypertension, is a condition in which the force of blood against the artery walls is too high.
The link between sleep apnea and high blood pressure is complex and multifaceted. Sleep apnea can cause repeated drops in blood oxygen levels, leading to increased blood pressure and strain on the cardiovascular system.
Additionally, the frequent awakenings and disrupted sleep caused by sleep apnea can also contribute to the development of high blood pressure.
Understanding the relationship between sleep apnea and high blood pressure is crucial for patients who have either condition.
If left untreated, both conditions can increase the risk of heart disease, stroke, and other health complications. Therefore, it is important to seek medical advice and treatment to manage both sleep apnea and high blood pressure.
Sleep Apnea and Blood Pressure
Sleep Apnea:
Obstructive sleep apnea syndrome is sleep disordered breathing that is characterized by frequent pauses in breathing or shallow breathing during sleep (hypopnea). It is a serious condition that can have significant effects on a person’s health and well-being.
There are two main types of sleep apnea: obstructive sleep apnea and central sleep apnea.
Obstructive sleep apnea is the most common type of sleep apnea. It occurs when the muscles in the back of the throat fail to keep the airway open during sleep. This causes breathing to stop and start repeatedly throughout the night.
Obstructive sleep apnea is often caused by obesity, but can also be caused by factors such as smoking, alcohol consumption, and certain medical conditions.
The symptoms of obstructive sleep apnea can vary, but may include loud snoring, gasping for air during sleep, waking up with a dry mouth or sore throat, morning headaches, difficulty concentrating, irritability, and daytime sleepiness. These symptoms can have a significant impact on a person’s quality of life, as well as their ability to function at work or in other daily activities.
Screening and Diagnosis of Obstructive Sleep Apnea:
Obstructive sleep apnea (OSA) occurs when the muscles in the back of the throat fail to keep the airway open during sleep, leading to interruptions in breathing and often causing the person to wake up gasping for air. While OSA can be a serious condition, it can be easily screened with questionnaires such as the Epworth Sleepiness Scale or Stop-BANG.
The Epworth Sleepiness Scale is a simple questionnaire that measures a person’s level of daytime sleepiness. The questionnaire asks the person to rate their likelihood of falling asleep during eight different daily activities, such as watching TV or reading. A score of 10 or higher on the Epworth Sleepiness Scale indicates a high likelihood of daytime sleepiness, which can be an indicator of OSA.
Similarly, the Stop-BANG questionnaire is a simple screening tool that can be used to assess a person’s risk of OSA. The questionnaire asks the person about their snoring habits, BMI, age, neck circumference, and other factors that can increase the risk of OSA. A score of 3 or higher on the Stop-BANG questionnaire indicates a high risk of OSA.
While questionnaires such as the Epworth Sleepiness Scale and Stop-BANG can be useful in screening for OSA, a definitive diagnosis requires a sleep study.
A sleep study can be conducted either in a sleep lab or at home, under the guidance of a physician. A sleep study involves monitoring the person’s breathing, heart rate, and other vital signs while they sleep, which can provide an accurate diagnosis of OSA.
If left untreated, sleep apnea increases the risk of a number of serious health problems. It has been linked to an increased risk of high blood pressure, heart disease, stroke, diabetes, and obesity. It can also increase the risk of accidents, as people with sleep disordered breathing are more likely to fall asleep while driving or operating heavy machinery.
High Blood Pressure:
High blood pressure, also known as hypertension, is a common condition in which the force of blood against the walls of the arteries is too high. This condition can lead to serious health problems, such as heart disease, stroke, and kidney failure.
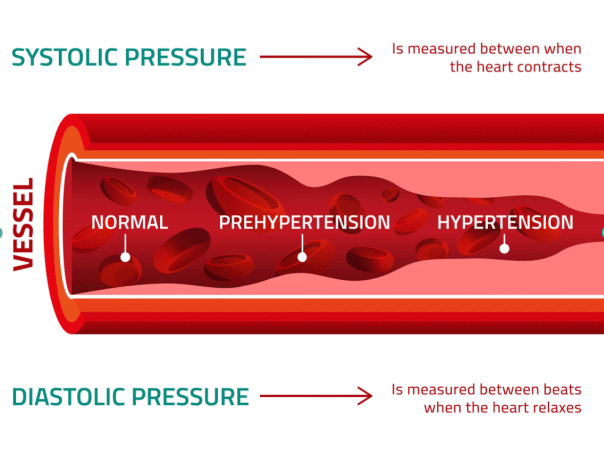
Blood pressure is measured using two numbers: systolic pressure, which measures the pressure in the arteries when the heart beats, and diastolic pressure, which measures the pressure in the arteries when the heart is at rest.
A blood pressure reading of 120/80 mm Hg or lower is considered normal. A reading between 120/80 mm Hg and 139/89 mm Hg is considered prehypertension, and a reading of 140/90 mm Hg or higher is considered hypertension. However, these numbers may vary depending on a person’s age, overall health, and other factors.

There are two main types of high blood pressure: primary (essential) hypertension and secondary hypertension. Primary hypertension is the most common type and is often caused by a combination of genetic and lifestyle factors, such as obesity, lack of physical activity, and a diet high in sodium. Secondary hypertension is caused by an underlying medical condition, such as kidney disease, hormonal disorders, or often, undiagnosed sleep apnea.
Symptoms of high blood pressure may not be noticeable at first, but over time, it can lead to symptoms such as headaches, dizziness, and nosebleeds. However, many people with high blood pressure have no symptoms at all, which is why it is often called the “silent killer.”
Treatment for high blood pressure typically involves lifestyle changes, such as eating a healthy diet, getting regular exercise, quitting smoking, and limiting alcohol intake. Medications, such as diuretics, ACE inhibitors, and beta-blockers, may also be prescribed to help lower blood pressure. It is important to work with a healthcare professional to determine the best treatment plan for individual needs.
In addition to lifestyle changes and medications, it is important for people with high blood pressure to monitor their blood pressure regularly and make changes to their treatment plan as needed. This may include adjusting medication dosages, changing medications, or making further lifestyle changes.
Linking Sleep Apnea and High Blood Pressure:
The link between obstructive sleep apnea and hypertension is believed to be due to the repeated episodes of oxygen deprivation that occur during obstructive sleep apnea. During an apnea episode, the brain sends a signal to the body to wake up and take a breath.
This causes a release of stress hormones, such as adrenaline, which can increase heart rate and blood pressure. Over time, these repeated episodes of oxygen deprivation and elevated blood pressure can lead to damage to the blood vessels and organs, including the heart and kidneys, and increase the risk of developing hypertension and other cardiovascular diseases.
The exact mechanisms by which obstructive sleep apnea leads to hypertension are not fully understood, but several hypotheses have been proposed. One theory is that obstructive sleep apnea causes chronic inflammation and oxidative stress, which can damage the endothelium, or lining, of the blood vessels and increase the risk of hypertension.
Another theory is that obstructive sleep apnea leads to changes in the autonomic nervous system, which regulates blood pressure, causing an imbalance that can lead to hypertension.
Several studies have demonstrated the link between obstructive sleep apnea as a risk factor for hypertension. In one study, researchers followed over 1,400 participants for up to 8 years and found that those with moderate to severe obstructive sleep apnea were more likely to develop hypertension than those without obstructive sleep apnea.
Another study found that treating patients with obstructive sleep apnea with continuous positive airway pressure (CPAP) therapy, which helps to keep the airway open during sleep, can significantly reduce blood pressure in people with both severe OSA, and hypertension.
Treatment of obstructive sleep apnea is important not only for improving sleep quality and reducing daytime symptoms but also for reducing the risk of hypertension and other cardiovascular diseases.

Lifestyle changes, such as weight loss, quitting smoking, and reducing alcohol intake, can help to reduce the severity of obstructive sleep apnea and improve blood pressure control. continuous positive airway pressure (CPAP) therapy is also an effective treatment option for obstructive sleep apnea and can lead to significant improvements in blood pressure control.
Sleep Apnea Forces the Heart to Work Harder
During an apnea episode, the body is deprived of oxygen, which triggers the release of stress hormones such as adrenaline and cortisol. These hormones cause an increase in heart rate and blood pressure, which in turn forces the heart to work harder.
Over time, the repeated episodes of oxygen deprivation and increased heart rate can lead to damage to the blood vessels and organs, including the heart, and increase the risk of cardiovascular disease.
The stress on the cardiovascular system caused by obstructive sleep apnea can also lead to changes in the structure and function of the heart.
Studies have shown that people with obstructive sleep apnea have an increased risk of developing left ventricular hypertrophy, which is a thickening of the heart muscle that can lead to heart failure.
Obstructive sleep apnea can also lead to changes in the blood vessels, including endothelial dysfunction, which can further increase the risk of cardiovascular disease.
The link between obstructive sleep apnea and cardiovascular disease is well established. In fact, people with obstructive sleep apnea are at an increased risk of developing hypertension, coronary artery disease, heart failure, and stroke.
In one study, researchers found that people with severe obstructive sleep apnea had a four times increased risk of developing heart failure compared to those without obstructive sleep apnea.
Another study found that people with obstructive sleep apnea who also had hypertension were at an increased risk of developing atrial fibrillation, a type of irregular heartbeat that can increase the risk of stroke and heart failure.
All About The Heart:
The heart is a muscular organ that is responsible for pumping blood throughout the body. It is located in the chest cavity, between the lungs, and is roughly the size of a closed fist. The heart is divided into four chambers: the right atrium, the right ventricle, the left atrium, and the left ventricle.
The right atrium receives deoxygenated blood from the body through the superior and inferior vena cavae. The blood then flows through the tricuspid valve into the right ventricle, which pumps the blood to the lungs for oxygenation. The left atrium receives oxygenated blood from the lungs through the pulmonary veins. The blood then flows through the mitral valve into the left ventricle, which pumps the blood out to the rest of the body through the aorta.
The heart works through a series of contractions and relaxations known as the cardiac cycle. During the contraction phase, or systole, the ventricles contract and push blood out of the heart. During the relaxation phase, or diastole, the ventricles relax and fill with blood from the atria. The heart rate, or the number of contractions per minute, is controlled by the sinoatrial node, a small bundle of cells located in the right atrium.
The heart interacts with the rest of the body through the circulatory system, which consists of the heart, blood vessels, and blood. The circulatory system is responsible for delivering oxygen and nutrients to the body’s tissues and removing waste products, such as carbon dioxide. The arteries carry oxygenated blood away from the heart, while the veins carry deoxygenated blood back to the heart. The capillaries, which are the smallest blood vessels, connect the arteries and veins and allow for the exchange of nutrients, oxygen, and waste products between the blood and the body’s tissues.
The heart is also closely connected to the nervous system, which controls the body’s involuntary functions, such as heart rate and blood pressure. The sympathetic nervous system, which is responsible for the “fight or flight” response, can increase heart rate and blood pressure in response to stress or danger. The parasympathetic nervous system, which is responsible for the “rest and digest” response, can decrease heart rate and blood pressure during periods of relaxation or sleep.
In addition to its role in the circulatory system, the heart also plays an important role in the endocrine system. The heart produces several hormones, including atrial natriuretic peptide (ANP), which helps to regulate the blood pressure levels and fluid balance in the body.
Consequences of the Heart Working Harder:
The repeated episodes of oxygen deprivation and increased heart rate that occur during both sleep apnea and hypertension episodes can cause changes in the structure and function of the heart, a leading risk factor for arrhythmias, heart failure, and stroke.
Arrhythmias are abnormal heart rhythms that can occur when the electrical impulses that regulate the heart’s contractions are disrupted. OSA can cause changes in the autonomic nervous system, which regulates heart rate and rhythm, leading to an increased risk of arrhythmias such as atrial fibrillation. Atrial fibrillation is a type of arrhythmia that can increase the risk of stroke and heart failure.
Heart failure occurs when the heart is no longer able to pump blood effectively to meet the body’s needs. OSA can cause changes in the structure of the heart, such as left ventricular hypertrophy, which can lead to heart failure. The repeated episodes of oxygen deprivation and increased heart rate can also cause damage to the blood vessels and organs, including the heart, increasing the risk of heart failure.
Stroke occurs when the blood supply to the brain is interrupted, either by a blood clot or a rupture in a blood vessel. OSA can increase the risk of stroke by causing changes in the blood vessels, such as endothelial dysfunction, which can increase the risk of blood clots. OSA can also cause changes in the autonomic nervous system, which can lead to high blood pressure, another risk factor for stroke.

Other cardiovascular consequences of OSA include hypertension, or high blood pressure, which can increase the risk of heart attack, stroke, and kidney disease. OSA has also been linked to an increased cardiovascular risk because of atherosclerosis, or the buildup of plaque in the arteries, which can increase the risk of heart attack and stroke.
The strain on the heart caused by sleep apnea can lead to a variety of health problems, including heart strain, cardiac arrhythmias, heart failure, and stroke.
Prevention and Treatment of OSA and Heart Disease:
Prevention of obstructive sleep apnea and heart disease involves addressing risk factors, such as obesity, smoking, and hypertension. Maintaining a healthy weight through a balanced diet and regular exercise can help to reduce the risk of OSA and heart disease.
Quitting smoking and limiting alcohol intake can also help to reduce the risk of these conditions. Managing medical conditions such as hypertension and diabetes can also help to prevent OSA and heart disease.
Treatment of OSA involves improving the quality of sleep and reducing the frequency and severity of apnea episodes. Continuous positive airway pressure (CPAP) therapy is the most effective treatment for OSA and has been shown to reduce the risk of cardiovascular disease. CPAP therapy helps to keep the airway open during sleep, which can reduce the number of apnea episodes and improve oxygen levels. Other treatments for patients with OSA can include weight loss, quitting smoking, and reducing alcohol intake.
Treatment of heart disease involves managing risk factors and reducing the workload on the heart. Lifestyle changes, such as a healthy diet, regular exercise, quitting smoking, and limiting alcohol intake, can help to improve heart health and reduce the various cardiovascular risk factors of heart disease. Antihypertensive medications, such as statins, beta-blockers, and ACE inhibitors, can also help to manage risk factors and improve heart health. In some cases, surgery or other procedures may be necessary to treat heart disease.
All About Hypertension
Definition:
Hypertension, also known as high blood pressure, is a common medical condition that affects millions of people worldwide. Hypertension is a leading risk factor for heart disease, which is the leading cause of death worldwide. It occurs when the force of blood against the walls of the arteries is consistently too high, which can lead to serious health problems such as heart disease, stroke, and kidney failure.
Blood pressure is measured using two numbers: the systolic pressure, which represents the force of blood when the heart contracts, and the diastolic blood pressure, which represents the force of blood when the heart is relaxed. A normal blood pressure reading is typically around 120/80 mmHg, with a systolic blood pressure of less than 120 and a diastolic pressure of less than 80.
Hypertension is diagnosed when a person’s blood pressure consistently measures at 140/90 mmHg or higher. However, blood pressure can vary throughout the day, so a diagnosis of hypertension typically requires multiple readings taken over several days or weeks.
Causes:
There are two types of hypertension: primary (or essential) hypertension and secondary hypertension. Primary hypertension is the most common type and has no identifiable cause. It is often related to risk factor such as a diet high in salt, lack of exercise, and obesity.
Secondary hypertension, on the other hand, is caused by an underlying medical condition such as kidney disease, thyroid problems, or an sleep related breathing disorder..
Symptoms:
While hypertension is a serious condition, it is often asymptomatic, meaning that people can have high blood pressure without even knowing it. Hypertension is often referred to as the “silent killer” because it typically does not have any noticeable symptoms.
However, some people with poorly controlled hypertension may experience common symptoms such as headaches, dizziness, and nosebleeds. This is why regular blood pressure checks are so important, especially as people age.
Diagnosis:
The diagnosis of hypertension is typically made through a blood pressure measurement. Blood pressure can be measured using a sphygmomanometer, which consists of an inflatable cuff that is placed around the upper arm and a pressure gauge. Additionally, ambulatory blood pressure monitoring and home blood pressure monitoring can be used to diagnose and monitor hypertension.
Complications:
Hypertension can lead to a variety of complications, including heart disease, stroke, kidney disease, vision loss, and sexual dysfunction.
Hypertension causes damage to the blood vessels, which can lead to the development of atherosclerosis and increase the risk of heart disease and stroke.
High blood pressure can cause the walls of the arteries to become thicker and stiffer, which can lead to a buildup of plaque and a narrowing of the arteries. This narrowing can reduce blood flow to vital organs such as the heart, brain, and kidneys, which can lead to damage and even failure of these organs.
In addition, hypertension can cause damage to the kidneys, leading to kidney disease and even kidney failure. Hypertension can also cause damage to the blood vessels in the eyes, leading to vision loss, and can impact sexual function.
Prevention and Treatment:
In addition to lifestyle changes such as reducing salt intake, increasing physical activity, and losing weight, medications are often used to manage hypertension. There are several classes of medications that can be used for blood pressure reduction, including diuretics, beta-blockers, ACE inhibitors, and calcium channel blockers. The choice of medication depends on the individual and their specific needs.
In some cases, lifestyle changes and medication may not be enough to manage hypertension, and additional treatments may be necessary. For example, people with resistant hypertension (hypertension that is difficult to control with medication) may benefit from procedures such as renal denervation, which involves using radiofrequency energy to disrupt the nerves that control blood pressure in the kidneys.
Conclusion
In conclusion, the link between obstructive sleep apnea and high blood pressure is a complex and multifaceted one that can have serious health implications if left untreated. If you have been diagnosed with either condition, it is important to seek medical advice and treatment to manage both and reduce your risk of developing complications.
At the same time, it’s crucial to remember that prevention is always better than cure. Make lifestyle changes such as losing weight, reducing salt intake, and quitting smoking to lower your risk of developing both obstructive sleep apnea and high blood pressure.