Pneumonia is a common yet potentially severe respiratory infection that affects millions of people worldwide. This comprehensive guide aims to demystify pneumonia by providing detailed information on its causes, symptoms, treatments, and preventative measures.
Understanding pneumonia is crucial for early detection and proper management of the condition.
Introduction to Pneumonia
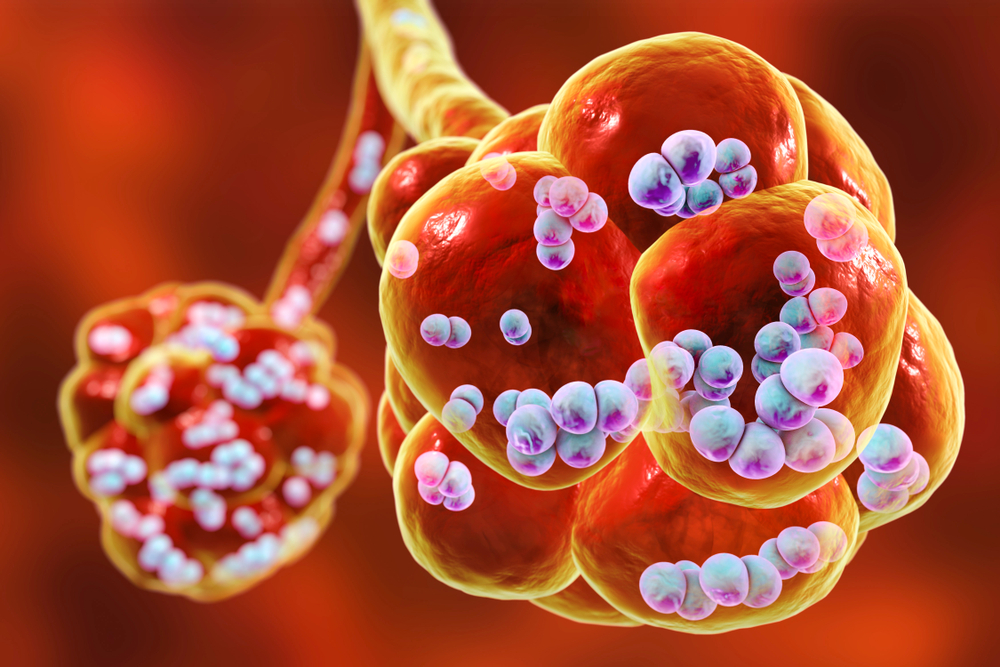
Pneumonia is an infection of one or both lungs, which causes inflammation and fluid build-up in the air sacs, or alveoli. This inflammation can make it difficult to breathe and can lead to various symptoms, some of which can be life-threatening.
By understanding pneumonia, you can take steps to prevent it and seek timely treatment if it does occur.
Different Types of Pneumonia
There are several types of pneumonia, categorized based on the cause of the infection.
Bacterial Pneumonia
Bacterial pneumonia is a type of pneumonia caused by various bacteria, with Streptococcus pneumoniae being the most common causative agent. Other bacteria, such as Haemophilus influenzae and Legionella pneumophila, can also cause this form of pneumonia.
Bacterial pneumonia typically presents with symptoms like high fever, productive cough with yellow or greenish sputum, shortness of breath, chest pain, and fatigue. The severity of these symptoms may range from mild to life-threatening, depending on factors such as the patient’s age, immune system, and overall health.
Unlike viral pneumonia, bacterial pneumonia can be effectively treated with antibiotics, which target and eliminate the bacteria responsible for the infection. Early diagnosis and prompt antibiotic treatment are crucial for successful recovery and reducing the risk of complications.
Preventive measures, such as vaccination against pneumococcal pneumonia and maintaining good hygiene, can help lower the risk of bacterial pneumonia.
Viral Pneumonia
Viral pneumonia is a type of pneumonia caused by various viruses, as opposed to bacteria or fungi. Common viral agents responsible for this form of pneumonia include the influenza virus, respiratory syncytial virus (RSV), and the novel coronavirus (COVID-19).
Viral pneumonia typically presents with symptoms such as fever, dry cough, shortness of breath, and fatigue, which may be similar to those experienced in bacterial pneumonia.
However, unlike bacterial infection, viral infection does not usually respond to antibiotic treatment. Instead, antiviral medications may be prescribed, depending on the specific virus causing the infection.
Supportive care, including rest, hydration, and over-the-counter fever reducers and pain relievers, can help alleviate symptoms and aid in recovery.
Prevention strategies include vaccination against certain viruses, maintaining good personal hygiene, and avoiding close contact with infected individuals.
Fungal Pneumonia
Fungal pneumonia is less common and occurs when fungi, such as Pneumocystis jirovecii, Aspergillus, or Cryptococcus, infect the lungs.
Fungal pneumonia is more likely to affect people with weakened immune systems, such as those with HIV/AIDS or those taking immunosuppressive medications.
Lobar Pneumonia
Lobar pneumonia is a type of pneumonia characterized by the inflammation and infection of a single lobe or section of the lung, rather than affecting multiple lobes or scattered areas throughout the lungs.
This form of pneumonia is most commonly caused by the bacterium Streptococcus pneumoniae. Lobar pneumonia typically presents with high fever, productive cough with rust-colored sputum, shortness of breath, and sharp chest pain that worsens during deep breaths or coughing.
As lobar pneumonia can progress rapidly and lead to severe complications if left untreated, prompt medical attention and appropriate treatment, usually involving antibiotics, are crucial for recovery.
In some cases, lobar pneumonia may be accompanied by pleural effusion, which is the accumulation of fluid between the layers of tissue that line the lungs and chest cavity, further complicating the condition and necessitating additional medical intervention.
Aspiration Pneumonia
Aspiration pneumonia occurs when food, liquids, or other foreign substances are accidentally inhaled into the lungs, causing an infection.
This type of pneumonia is more common in people with difficulty swallowing or impaired cough reflexes, such as stroke victims or those with neurological disorders.
Walking Pneumonia
Walking pneumonia, also known as atypical pneumonia or mycoplasma pneumonia, is a milder form of pneumonia that generally does not require hospitalization.
This type of pneumonia is typically caused by the bacterium Mycoplasma pneumoniae, which results in less severe symptoms compared to more serious cases of pneumonia.
Patients with walking pneumonia may experience milder symptoms such as a dry cough, low-grade fever, mild chest pain, and fatigue. These symptoms often resemble those of a common cold, leading people to continue their daily activities without realizing they have a lung infection – hence the term “walking” pneumonia.
Despite its milder nature, it is still essential to seek medical attention and receive appropriate treatment, such as antibiotics, to ensure a full recovery and prevent potential complications.
Hospital Acquired Pneumonia
Hospital-acquired pneumonia, also known as nosocomial pneumonia or healthcare-associated pneumonia, is a type of pneumonia that occurs in patients during their stay in a hospital or other healthcare facility.
This form of pneumonia is particularly concerning as it often involves antibiotic-resistant bacteria, making it more challenging to treat.
Patients who are on mechanical ventilation, have weakened immune systems, or have underlying chronic health conditions are at a higher risk of developing hospital-acquired or ventilator associated pneumonia.
Strict infection control measures, including proper hand hygiene, sterilization of medical equipment, and adherence to isolation protocols, are essential to prevent the spread of hospital-acquired pneumonia and protect vulnerable patients.

Recognizing Pneumonia Symptoms
The symptoms of pneumonia can vary in severity and frequency. Early recognition is crucial for timely treatment and better outcomes.
Pneumonia Risk Factors
Certain factors can increase the risk of developing pneumonia, including:
Age: Young children and older adults are more susceptible due to weaker immune systems.
Pre-existing health conditions: Chronic lung diseases, heart conditions, and diabetes and a weakened immune system, elevate the risk of pneumonia.
Lifestyle factors: Smoking and excessive alcohol consumption weaken the immune system and damage the lungs.
Environmental factors: Exposure to air pollution, chemical fumes, or dust irritates the lungs, increasing the risk of pneumonia.
Common Symptoms
Cough, often producing mucus
Fever
Shortness of breath
Chest pain when breathing or coughing
Fatigue and weakness
Loss of appetite
Less Common Symptoms
Sweating and chills
Confusion or disorientation, especially in older adults
Headache
Muscle aches
Rapid breathing and heart rate
Severe Pneumonia Symptoms
Bluish lips or nails due to low oxygen levels
Severe difficulty breathing
Persistent high fever
Rapid heart rate and chest pain
Confusion, disorientation, or lethargy
The Four Stages of Pneumonia
Pneumonia typically develops in four stages:
Congestion: During this stage, the lungs become congested with fluid and inflammatory cells, leading to difficulty breathing and reduced oxygen levels.
Consolidation: Inflammation and fluid accumulation in the lungs worsen, and the affected lung tissue becomes solidified.
Resolution: As the infection subsides and the immune system fights the infection, the lungs begin to clear, and symptoms start to improve.
Recovery: The inflammation and fluid in the lungs resolve, and lung function gradually returns to normal.
Diagnosing Pneumonia
A healthcare professional will diagnose pneumonia based on a combination of a physical examination and diagnostic tests.
Physical Examination
To confirm a pneumonia diagnosis, one or more of the following tests may be performed:
Imaging tests: Chest X-rays or CT scans can reveal areas of inflammation in the lungs.
Blood tests: Blood tests can help determine the cause of the infection and assess the severity.
Sputum tests: Analyzing a sample of mucus (sputum) coughed up from the lungs can help identify the specific organism causing the infection.
Diagnostic Tests
To confirm a pneumonia diagnosis, one or more of the following tests may be performed:
Imaging tests: Chest X-rays or CT scans can reveal areas of inflammation in the lungs.
Blood tests: Blood tests can help determine the cause of the infection and assess the severity.
Sputum tests: Analyzing a sample of mucus (sputum) coughed up from the lungs can help identify the specific organism causing the infection.
Pleural fluid culture: examines a sample of fluid that has collected in the pleural space to evaluate infection or determine the cause of fluid buildup in the pleural space.
Pneumonia Treatment Options
Treatment for pneumonia depends on the type and severity of the infection, as well as the patient’s overall health.
Home Remedies and Self-Care
For mild cases of pneumonia, the following self-care measures can help:
Get plenty of rest to allow your body to heal
Stay hydrated by drinking water, clear fluids, or warm beverages
Take over-the-counter pain relievers and fever reducers, such as ibuprofen or acetaminophen, to manage symptoms
Use a humidifier or take steamy showers to help ease breathing
Medical Treatments
Depending on the causes of pneumonia, a healthcare provider may prescribe:
Antibiotics to treat bacterial pneumonia
Antiviral medications to treat viral pneumonia
Antifungal medications to treat fungal pneumonia
In some cases, additional medications such as bronchodilators or corticosteroids may be prescribed to improve breathing and reduce inflammation.
Hospitalization
Severe pneumonia or cases with complications may require hospitalization. In the hospital, treatment may include:
Intravenous (IV) antibiotics, antivirals, or antifungals
Oxygen therapy to increase oxygen levels in the blood
Respiratory therapy, including the use of a nebulizer or mechanical ventilation for severe breathing difficulties

Preventing Pneumonia
Taking steps to prevent pneumonia is essential, especially for those at higher risk or who have a weakened immune system.
Vaccination
Vaccines are available to protect against some of the most common causes of bacterial pneumonia and viral pneumonia, such as pneumococcal, Haemophilus influenzae type b (Hib), and seasonal flu vaccines.
Talk to your healthcare provider about which vaccines are appropriate for you.
General Health and Hygiene
Maintaining a healthy lifestyle can help strengthen your immune system and reduce the risk of pneumonia:
Wash your hands frequently with soap and water, or use hand sanitizer when handwashing is not possible.
Avoid close contact with people who are sick.
Practice good oral hygiene to reduce the risk of aspiration pneumonia.
Maintain a balanced diet, exercise regularly, and get enough sleep to support a healthy immune system.
Environmental Factors
Reducing exposure to lung irritants can help prevent pneumonia:
Avoid smoking and exposure to secondhand smoke.
Minimize exposure to air pollution, chemical fumes, and dust.
Wear a mask in environments with high levels of irritants or when exposed to contagious respiratory illnesses.
Pneumonia Complications
Pneumonia can lead to complications, including:
Respiratory failure
Sepsis, a life-threatening infection that can spread throughout the body
Lung abscess, a pus-filled cavity that develops within the lung tissue
Pleural effusion, an accumulation of fluid between the layers of tissue that line the lungs and chest cavity
Acute respiratory distress syndrome (ARDS)
To reduce the risk of complications:
Seek prompt medical attention if you suspect pneumonia
Follow your healthcare provider’s instructions for treatment and medication
Monitor your symptoms and report any worsening or new symptoms to your healthcare provider
Pneumonia FAQs
How long does it take to recover from pneumonia? Recovery time varies depending on the type and severity of pneumonia, as well as the individual’s overall health. Most people start feeling better within a week or two, but it can take a month or longer for a full recovery.
Can pneumonia be contagious? Viral and bacterial pneumonia can be contagious, spreading through respiratory droplets from coughing, sneezing, or close contact with an infected person. Fungal pneumonia is generally not contagious.
Are there any long-term effects of pneumonia? Most people recover completely from pneumonia without lasting effects. However, in some cases, pneumonia can cause lasting damage to the lungs, leading to chronic respiratory issues and other chronic health problems.
Can you get pneumonia more than once? Yes, it is possible to have pneumonia diagnosed more than once. Being vaccinated and taking preventative measures can reduce your risk of recurrent pneumonia.
What is the difference between pneumonia and bronchitis? Both pneumonia and bronchitis are infections of the respiratory system, but they affect different parts of the lungs. Pneumonia is an infection of the air sacs (alveoli), while bronchitis is an inflammation of the bronchial tubes that carry air to and from the lungs.
ConclusionPneumonia, a common respiratory infection, affects millions of people worldwide. It occurs when the air sacs in one or both lungs become inflamed and filled with fluid, making it difficult to breathe.
The causes of pneumonia include bacteria, viruses, and fungi, with Streptococcus pneumoniae being the most frequent offender in adults.
While anyone can develop pneumonia, young children, older adults, and those with chronic health conditions or weak immune systems have increased risk.
Recognizing the symptoms of pneumonia, such as cough, fever, shortness of breath, and chest pain, is crucial for timely treatment and is vital to avoid serious complications.
As pneumonia progresses, it goes through four stages: congestion, consolidation, resolution, and recovery.
During these stages, the lungs become congested, inflamed, and solidified before gradually returning to normal. To diagnose pneumonia, healthcare professionals rely on physical examinations and various diagnostic tests like chest X-rays and blood tests.
Treatment for viral and bacterial pneumonia depends on the type and severity of the infection. For milder cases, home remedies and self-care, like getting plenty of rest and staying hydrated, can help alleviate the symptoms of pneumonia.
Medical treatments may include antibiotics, antivirals, or antifungals, depending on the cause of the infection. In severe cases, hospitalization may be necessary.
Preventing pneumonia involves vaccination, maintaining good health and hygiene, and reducing exposure to lung irritants.
By understanding the causes, symptoms of pneumonia, and treatments of pneumonia, and taking preventive measures, you can reduce your risk of developing this common respiratory disease and its potential complications which include respiratory failure.
Stay informed, stay healthy, and don’t forget to give a like if you find this information helpful!